Many people today face the challenge of missing teeth or a damaged tooth. This can make eating, speaking, and smiling feel hard. If you’re looking for a solution, understanding what is dental implants might be your first step.
Dental implants provide a solution for replacing missing teeth with ones that look and work like natural teeth.
Dental implants are made of titanium and act as artificial roots for teeth when inserted into the jawbone. They support new artificial teeth where your own were once located. In this article, we’ll guide you through the types of dental implants, how the procedure works, and its impact on oral health.
Keep reading to learn more about this long-term solution for replacing missing teeth.
What are Dental Implants and How Do They Work?
Transitioning from the introduction to dental implants, it’s essential to understand what these innovations are and their functionality in oral health. A dental implant acts as a robust foundation for either fixed or removable replacement teeth that look like your own natural teeth.
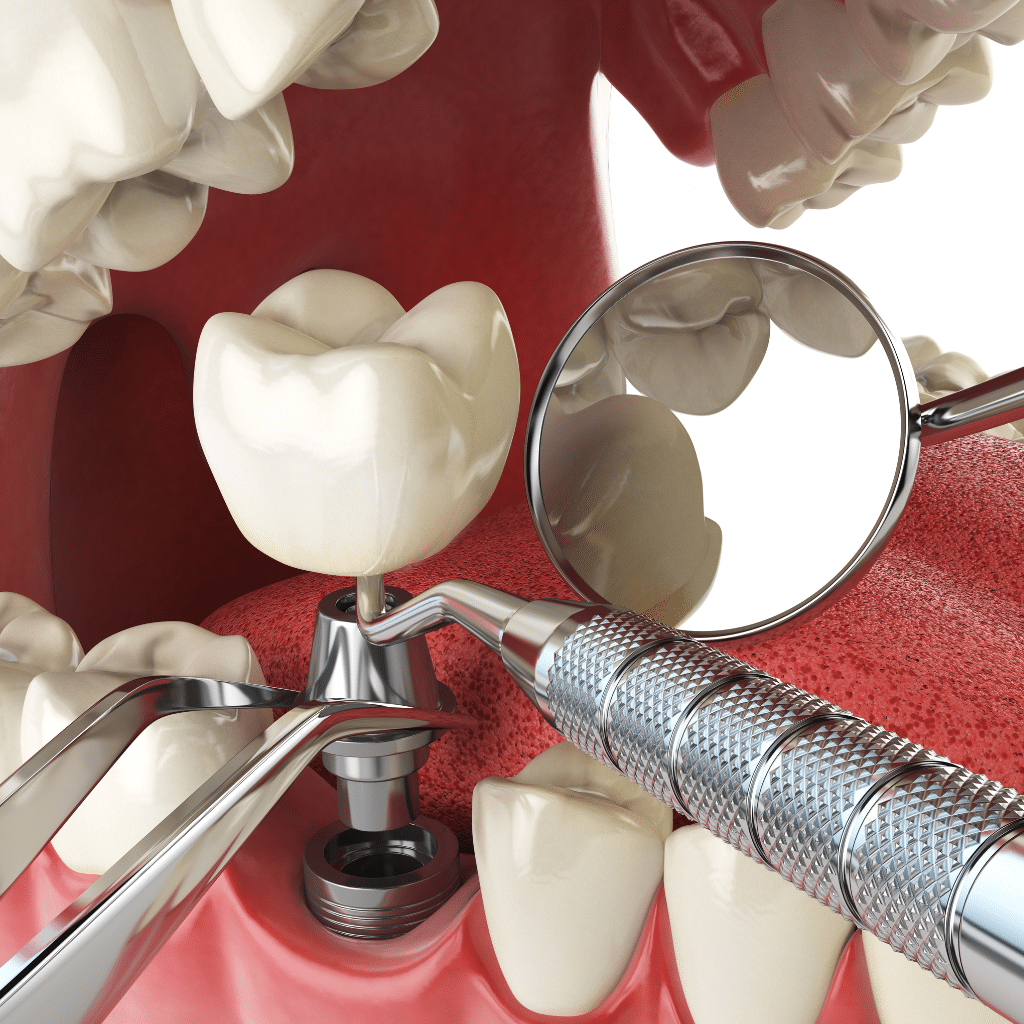
Surgeons insert these implants into the jawbone, where they fuse with bone over several months, a process known as osseointegration. This fusion creates a stable support for new artificial teeth.
Dental implants merge with your bone; they become part of you, explains Dr. Suresh Mohan Kumar. The procedure involves minor surgery at the implant site, where maxillofacial surgeons place a titanium post inside the jawbone under local anesthesia. Titanium is chosen for its compatibility with the human body and ability to bond with bone without being recognized as a foreign object. Once healed, this post serves as an anchor for attaching abutments and crowns or dentures, providing patients not just aesthetic satisfaction but functional benefits similar to real teeth.
Definition of a Dental Implant
A dental implant acts as a foundation for false teeth, such as crowns, bridges, or dentures. It’s made to act just like a real surgically placed artificial tooth root in the jawbone.
Dental implants are mostly crafted from titanium. This metal works well with the human body and helps to anchor the new artificial tooth in place securely. The success of an implant depends on its ability to integrate with the bone through a process called osseointegration.
Over several months, this integration makes the implant stable enough to support one or more artificial teeth.
These implants have transformed how missing or damaged teeth are treated, offering a long-term solution compared to traditional options like dentures or bridges. Whether it’s replacing one tooth or several teeth or providing support for removable dentures, dental implants improve oral health by maintaining bone structure and reducing bone loss.
They also help in preserving the natural shape of your face and smile.
How Implants Are Surgically Placed in the Jawbone
Dental implant surgery follows a series of steps to securely place the implant into the jawbone, where it will serve as the base for the new tooth. First, dentists ensure that there is enough bone to support the implant.
If not, they may perform minor bone grafting. This process gives a strong foundation for the implant. After preparing the jawbone, they make an incision in the gum tissue to reveal the bone area where they want to place the implant.
Next, dental surgeons carefully drill holes into the bone, where they will insert metal posts that act as roots for artificial teeth. These implants are made of titanium because they fuse well with bone tissues through a process called osseointegration.
Over time, this connection between titanium and jawbone builds a sturdy base for setting up crowns or bridges on top of these implants. This step ensures that replacement teeth feel and function like natural ones without affecting other teeth around them.
The focus then shifts to understanding how titanium plays a crucial role in dental implants.
The Role of Titanium in Dental Implants
Titanium plays a crucial role in the success of most dental implants. Due to its strength and biocompatibility, titanium enables osseointegration, during which the implant bonds with the jawbone.
This process is vital for the stability of the implant and supports a dental crown, bridge, or denture on top. Titanium’s ability to bond with bone makes it an ideal material for long-term tooth replacement solutions.
Surgeons choose titanium because it rarely causes reactions in the body. This minimizes the risk of infection and supports healing around the implant site. The metal’s durability means that once placed, a titanium implant can last many years with proper care and maintenance.
Its reliability has made titanium the go-to choice for replacing missing teeth among healthcare professionals worldwide.
What is the Dental Implant Procedure Like?
The dental implant procedure starts with a comprehensive evaluation of your mouth and teeth to ensure you’re a good candidate. Your dentist or oral surgeon will take detailed X-rays and possibly 3D images to plan the exact placement of the implant.
During surgery, they will carefully insert the titanium implant into your jawbone, which acts as a new root for the tooth. This step requires precision to avoid complications and ensure success.
After placing the implant, you’ll need time to heal; this period allows the jawbone to grow around the implant in a process known as osseointegration. It can take several months. Once healed, an abutment is attached to serve as a base for your new tooth.
Finally, a custom-made crown that blends seamlessly with your natural teeth is placed on top of the abutment.
A successful dental implant feels and functions like your own teeth.
Post-surgery care involves practicing good oral hygiene by brushing, flossing regularly, and keeping follow-up appointments with your dentist. Eating soft foods initially helps prevent infection while healing occurs around where they worked on your mouth during surgery.
Steps Involved in Dental Implant Surgery
Acquiring a dental implant comprises crucial stages. Each stage is vital for the implant’s success and your overall oral health.
- Dental specialist consultation: Start your journey with an appointment with your dentist or an oral and maxillofacial surgery specialist. They will assess your medical conditions, discuss treatment alternatives, and decide if implants are suitable for you.
- Comprehensive dental examination: You will undertake an exhaustive assessment that includes dental X-rays and possibly creating models of your teeth and mouth.
- Treatment planning: After considering factors like the number of teeth you’re missing and the state of your jawbone, the dentist will devise a custom treatment plan. This could involve other procedures, such as gum care or bone grafting if required.
- Bone grafting (if necessary): If your jawbone is too soft or insufficiently thick, bone grafting might be needed to provide secure support for the implant.
- Dental implant placement: During this surgery, the dentist cuts into your gum to expose the bone, then drills holes into the bone where they will insert the metal post, the implant’s main component. It acts as the new root for your artificial tooth.
- Healing and bone growth: Post implant placement, osseointegration initiates. This process involves your jawbone growing into and uniting with the dental implant’s surface—a vital phase that could take a few months.
- Abutment attachment: Once healing is completed, another minor surgery is conducted to attach an abutment—the component where the crown will be attached eventually—to each implant.
- Creating and attaching new teeth: Dental crowns, designed to mimic your natural teeth, are fastened to the abutments. Adjustments in fit and color matching are made in this final stage for a natural look.
- Post-surgery care: Your dental team will give directions on how to care for implants at home post each surgical stage, which includes managing discomfort with prescribed medications or over-the-counter pain relievers and ensuring cleanliness through proper hygiene practices.
This thorough approach guarantees that every patient receives custom care suited to their unique needs while sustaining high safety standards throughout all dental implant surgery stages.
What to Expect During the Surgical Procedure
Moving from understanding the steps involved in dental implant surgery, let’s discuss what takes place during the surgical procedure. The dentist or oral surgeon will start by numbing the area with local anesthesia to ensure you feel no pain during the operation.
They then make a small incision in your gum to expose the jawbone where they drill a hole for placing the implant. This process requires precision to avoid damage to adjacent teeth and ensure proper alignment.
After inserting the implant into your jawbone, your dentist may attach a temporary denture for cosmetic purposes until healing is complete and you’re ready for permanent replacement teeth.
The entire procedure can last several hours but varies based on how many implants are required. Post-operation, it’s normal to experience some swelling and discomfort, but this typically subsides within a few days of proper care and as prescribed medication by your healthcare provider.

Post-Surgery Care and Recovery
Caring for your gums and teeth after dental implant surgery is crucial to ensure the success of the implant. Right after the procedure, it’s important to follow all the guidance provided by your dental care team.
This involves taking prescribed medications to control pain and prevent infection. Eating soft foods helps avoid stress on your new implants during the initial healing phase.
The first few days post-surgery are vital for a patient’s recovery emphasizes Dr. Suresh Mohan Kumar. Keeping the surgical site clean while avoiding direct contact can aid in faster healing. Regular check-ups with your dentist or oral surgeon allow them to monitor healing and address any concerns early on, ensuring implants remain healthy and properly integrate with the jawbone over time.
What Types of Implants Are Available?
Patients can choose from several types of dental implants based on their needs. Endosteal implants are the most common type. They go directly into the jawbone, providing strong support for artificial teeth.
For those who might not have a healthy jawbone and wish to avoid bone grafting, subperiosteal implants offer an alternative. These rest on top of the jawbone but under the gum.
Another option includes mini dental implants (MDIs). MDIs are thinner than traditional ones and are often used to stabilize lower dentures. This variety can be especially helpful for patients looking for less invasive options or those with minimal bone mass.
Each type has its unique benefits and applications, enabling personalized treatment plans that cater to various dental conditions and preferences. Dentists assess each patient’s situation to recommend the best implant system that will support dental restoration effectively, offering a long-term solution for missing teeth.
Different Types of Implants for Various Needs
Dental implants are available in various types to meet different needs, ensuring a solution that works best for each patient. Endosteal implants are the most common type, placed directly in the jawbone and serving as a strong foundation for artificial teeth.
For patients who do not have a healthy jawbone and cannot undergo a bone augmentation procedure, subperiosteal implants offer an alternative by sitting on top of the jawbone under the gum tissue.
Mini dental implants (MDIs) are smaller than traditional ones and often used to stabilize lower dentures. This option requires less bone structure and can be less invasive, making it ideal for patients seeking a quicker recovery.
Another innovative approach involves All-on-4® implants, designed to support all teeth with just four implants strategically placed in areas of higher bone density. Understanding these options helps individuals make informed decisions about replacing missing teeth or securing dentures effectively, leading to improved oral health and comfort.
Choosing the Right Type of Implant for You
Exploring different types of implants reveals there’s one suited for every unique need. Making the right choice depends on several factors including your jawbone health, any existing health conditions, and your expectations from your dental treatment.
It is crucial to understand that different implants function differently and offer varied benefits. Some are meant for replacing a missing tooth, while others support a dental bridge or dentures if you’re missing several teeth.
Your smile should receive individualized care, ensuring that the selected implant meshes well with your natural teeth.
Evaluating your options requires a consultation with a dental specialist who can assess your oral health and suggest the implant type most suitable for you. Whether a single implant is required for one missing tooth or multiple implants to support the teeth and gums fully, each decision contributes to achieving the best possible outcomes with long-term solutions in mind.
The process may require several visits, but picking the right type ensures both durability and compatibility with healthy teeth surrounding the implant site.
Understanding Implant Systems
After choosing the right type of implant for you, understanding implant systems becomes vital. Implant systems consist of several components that work together to replace missing teeth.
These include the implant body, which surgeons place in the jawbone, and the abutment, which attaches to the implant body above the gum line. The final piece is a crown or artificial tooth that attaches to the abutment.
Implant bodies are made from titanium because they integrate well with bone, creating a stable support for dental implants. This base allows patients to chew and speak without issues typically caused by less reliable treatments like dentures.
Each system is designed keeping in mind long-term solutions for oral health and functionality. Knowing how these elements fit together helps in making an informed decision about getting dental implants as a treatment option for missing teeth.
How Safe and Successful Are Dental Implants?
Dental implants have a success rate of 95% over ten years, making them a reliable long-term solution for replacing missing teeth.
Implants are made from titanium, which bonds well with human bone. The process of attaching the abutment and implant requires precision, ensuring that each step supports a dental implant effectively.
Patients can feel confident in this procedure’s safety as it follows rigorous standards set by clinical implant dentistry.
Safety concerns for dental implants are minimal when performed by experienced dentists. Proper evaluation and tests before surgery help identify any potential risks to tailor the treatment accordingly.
Dental implants replace teeth without affecting neighboring ones, preserving oral health and preventing decay and jawbone loss since implants mimic natural teeth roots. They offer both functional and aesthetic benefits, making them an excellent choice for those seeking to restore their smile confidently.
Success Rates and Implant Failure Risks
Dental implants have high success rates, offering a long-term solution for missing teeth. Studies show that these implants succeed in over 95% of cases. This means most patients enjoy the benefits without issues.
Implants work well because they fuse to your jawbone, forming a strong base for the replacement tooth.
However, like any surgical procedure, there are risks of implant failure. Risks may increase if the patient smokes or has certain health conditions such as diabetes. Proper care and maintenance can lower these risks significantly.
Doctors test each implant carefully to ensure it supports a dental implant effectively before proceeding with surgery. If an implant does fail, dentists can often replace it, ensuring that patients still have access to reliable dental solutions.
Ensuring the Success of the Implant
To ensure the success of a dental implant, patients must follow their dentist’s instructions closely. Good oral hygiene plays a crucial role. Brushing twice a day and flossing daily can prevent infections that might jeopardize the implant.
Regular check-ups allow dentists to catch any potential issues early on.
Patients should also avoid habits that could harm the implant, like smoking or chewing hard foods. Keeping up with these practices supports the health of the surrounding teeth and jawbone.
Such diligence ensures implants remain healthy and functional for years to come.
Are Dental Implants Safe for Everyone?
Dental implants are a long-term solution for replacing missing teeth and have high success rates. They offer a stable base for the implant, effectively supporting dental prosthetics like crowns, bridges, or dentures.
Most people who need to replace a missing tooth can safely get dental implants. The process involves placing a titanium surface into the jawbone, which fuses with bone over time.
However, not everyone is an ideal candidate for dental implants. Patients with certain health conditions, such as uncontrolled diabetes, severe gum disease, or those undergoing radiation therapy in the head or neck area, may face higher risks during and after surgery.
A thorough pre-surgery evaluation by a dentist is critical to determine if dental implants are suitable for you. This includes discussing your medical history and possibly conducting tests to ensure your jawbone can support an implant effectively.
What Should I Do Before Getting a Dental Implant?
Visiting a dentist or dental specialist is the initial stage before receiving a dental implant. They will examine your oral health to verify that your gums and jawbone are capable of supporting a dental implant.
This may entail X-rays or 3D scans to check bone density and structure. Your dentist will also confirm whether any initial procedures, such as gum treatment or bone grafting, are necessary to be ready for the installation of a dental implant.
It’s also vital to comprehend the expenses and services involved. Dental implants necessitate a commitment of money as well as time. Your specialist will detail the full cost, encompassing the surgery itself, the abutment, and the crown that takes the place of lost teeth.
They’ll further clarify the number of trips required for a full recovery and the maintenance your new tooth will require to retain its health and function over time.
Consulting with a Dentist or Dental Specialist
Consulting with a dentist or dental specialist is essential before you decide on getting dental implants. They will review your oral health to make sure implants are the right choice for you.
This may include evaluating if your gums are healthy and if there’s enough bone to support the implant. If they find issues, such as weak bone structure, they may recommend treatments to improve your candidacy for an implant.
Your dentist will also explain how many implants you might need based on the number of teeth missing. For example, if you’re missing at least one tooth, one implant might be enough.
However, more extensive gaps may require several implants. Understanding the process helps set realistic expectations about surgery and recovery times.

Pre-Surgery Evaluations and Tests
Before undergoing the placement of a dental implant, patients undergo several important evaluations and tests. These steps ensure that dental implants are a healthy choice for you.
- Dental and Medical History Review: Your dentist will first gather detailed information about your oral and general health history. This step highlights any conditions that might affect the success of the implant procedure.
- Oral Examination: A detailed examination of your mouth checks the health of your gums and the strength of your jawbone. The dentist looks for signs that support a dental implant.
- Imaging Tests: X-rays or CT scans provide images of your jawbone. These help in planning the procedure by showing where to place the dental implant.
- Impressions: Taking impressions of your mouth allows for the creation of a model. This model helps in understanding how your teeth fit together.
- Evaluation for Dentures or Braces: If you currently wear dentures or braces, the dentist will assess how these might influence implant placement and success.
- Discussion on Number of Implants Required: Depending on your need, whether it’s replacing one tooth with a dental implant or several, the dentist determines how many implants are needed.
- Bone Density Test: This test checks if your jawbone can support a dental implant firmly. Sometimes, additional treatments may be required to improve bone density.
- Treatment Plan Development: After all evaluations, a customized plan is made outlining what needs to be done before, during, and after surgery.
- Cost Estimation: You receive an estimate covering all aspects from pre-surgery evaluations to post-surgery care, including any necessary follow-up visits.
- Consent Form Review and Signing: Finally, you go through consent forms detailing risks and benefits, enabling you to make an informed decision about moving forward with the surgery.
Understanding the Costs and Services Involved
Dental implant procedures vary widely in cost, depending on the type of implant and surgery needed. Patients often wonder about the price before getting implants. The expenses cover not just the actual implant but also include pre-surgery evaluations and tests.
Dentists use these evaluations to make sure implants are healthy for your jawbone and gums. Knowing these costs upfront helps you plan better for this long-term solution.
The services involved go beyond just placing the implant into your jawbone. They encompass initial consultations, any necessary oral surgery to prepare your bone structure, and follow-up care to ensure the success of the procedure.
Each step plays a crucial role in replacing teeth with durable implants made to last for years, giving you a clear understanding of what financial investment is required for maintaining optimal oral health through dental implants.
Conclusion
Understanding the costs and services involved creates clear expectations before initiating the process for dental implants. This durable solution to replace absent teeth boasts remarkable success rates, validating it as a dependable option for many.
Dental implants do more than enhance appearances; they dramatically contribute to oral health by thwarting jawbone deterioration and stabilizing nearby teeth.
Patients contemplating this treatment should diligently appraise their choices and discuss with dental experts to affirm it fits their requirements. Success is dependent on comprehensive pre-surgery evaluations, knowing how to care post-surgery, and selecting the correct implant system.
With adequate strategizing and care, dental implants can successfully revive smiles, proving them a valuable investment in personal oral health.


